As health communicators, we know that the best way to keep COVID-19 from spreading is (still!) to stay home. But we also know that with states and communities reopening, people will be venturing out more — and that means it’s time to talk about harm reduction.
In the case of COVID-19, of course we’ll continue to tell people that the safest choice is to stay home. But we also need to help people stay safer when do they go out.
And we need to acknowledge that for many people, staying home isn’t an option. Essential workers — and now, in many states, non-essential workers — have to leave their homes or risk losing their paychecks.
People nationwide are also heading out to protest another public health crisis: systemic racism and police violence. And while we can’t eliminate their risks entirely, we can help them stay safer.
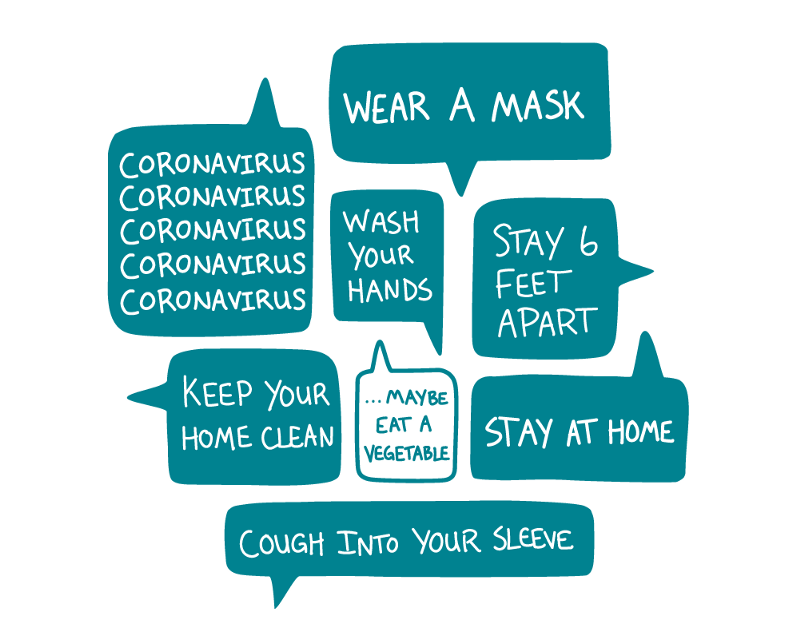
So share these tips to help people protect themselves and others whenever they leave their homes — no matter the reason:
- Stay outside. Studies have found that people are much less likely to get COVID-19 when they’re outdoors. That makes parks and backyards far better choices than bars or malls.
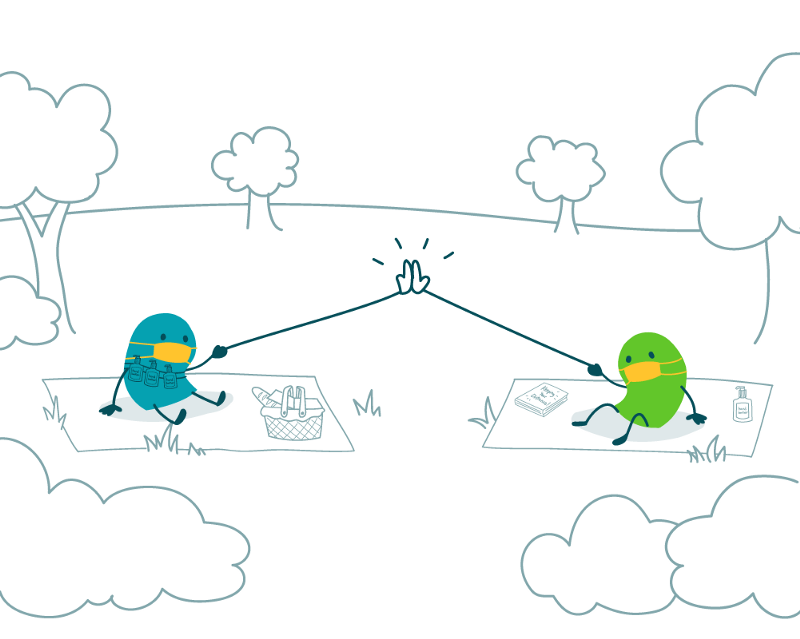
- Keep your distance. Since the early days of the pandemic, public health experts have advised everyone to stay at least 6 feet away from people they don’t live with — and that guidance hasn’t changed. Two friends meeting up at the park, for example, are better off sitting several feet apart in the grass than rubbing elbows on a park bench.
- Keep it quick. Researchers think that the longer you’re around someone who has COVID-19, the higher your risk of getting infected. That means popping into a restaurant for a few minutes to grab takeout is less risky than sitting inside for an hour while you eat dinner.
- Keep it small. Spending time in a crowd — think parties, concerts, or packed restaurants — is a bad idea (even outdoors!). It’s hard to keep your distance from others, and more people means a higher risk that one of those people could have the virus. So keeping gatherings very small can help.
- Wear a mask — and stay away from people who aren’t wearing them. Evidence shows that wearing a cloth mask helps stop people from spreading COVID-19 to others. And since people without symptoms can still be contagious, everyone needs to wear masks whenever they can’t keep their distance.
- Wash your hands. A lot. Use hand sanitizer if there’s no soap and water available. And don’t touch your face. Sound familiar? That’s because tips for “practicing good hygiene” still apply, whether you’re at home or out and about.
As always, be sure to adapt these tips to fit your specific audience. Harm reduction might look a lot different for certain groups, like people who are experiencing homelessness. So remember to keep your audience front and center when you’re developing health comm products — that’s always part of our job, but it’s especially important now.
The bottom line: People won’t stay home indefinitely — so offer practical advice to help them lower their risk of catching or spreading COVID-19 when they do go out.